Wound healing is a remarkable process that the body undergoes to repair itself after an injury. It involves a series of complex steps that work together to promote healing and restore the integrity of the skin. Understanding how wounds heal is important for fighters who may sustain injuries during combat or training. By knowing the stages of wound healing and the appropriate wound care treatments, fighters can optimize their recovery and minimize the risk of complications.
- Wound healing is a complex process that involves multiple stages.
- The stages of wound healing include stopping the bleeding, inflammation, growth and rebuilding, and strengthening.
- Factors such as reduced blood supply and infection can delay the healing process.
- Proper wound management and timely medical attention are crucial for optimal healing.
- Advancements in wound healing techniques and treatments have improved outcomes in recent years.
The Basic Steps of Wound Healing
The process of wound healing involves several essential steps that work together to restore the integrity of the skin. Understanding these steps is crucial for optimizing recovery and minimizing complications. Let’s explore how wounds heal on the body.
Stopping the Bleeding
When the skin is cut or punctured, the first step in wound healing is stopping the bleeding, also known as hemostasis. Blood cells clump together to form a clot, creating a protective barrier that prevents further blood loss and allows the healing process to begin.
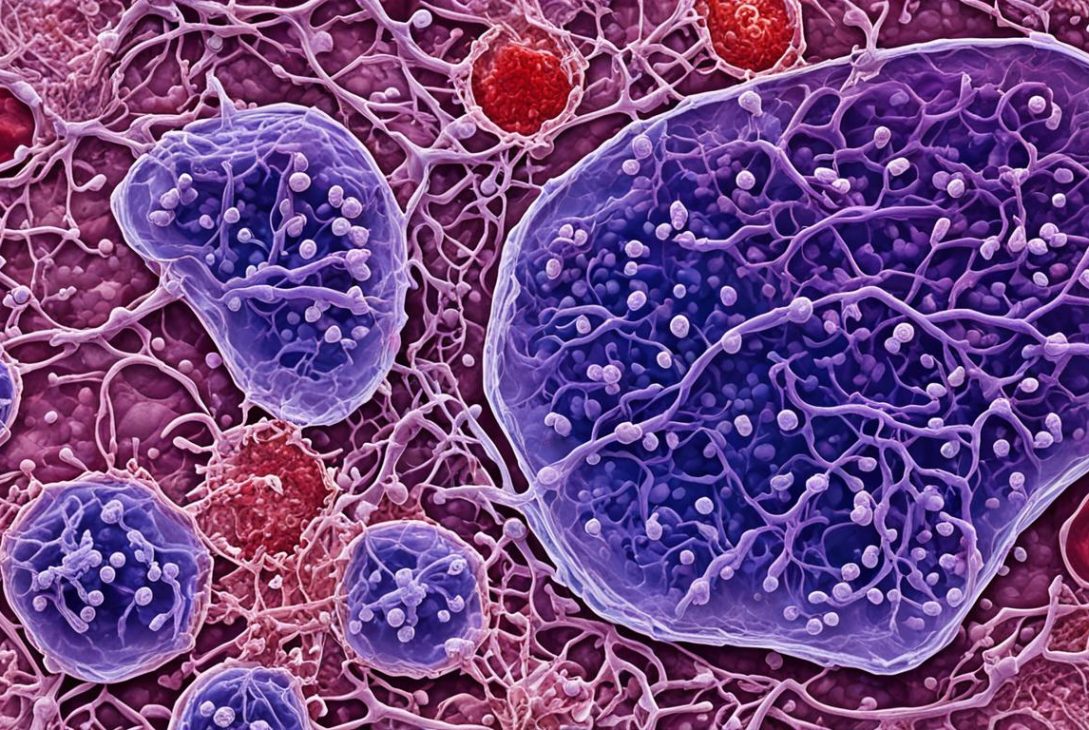
Inflammation
Inflammation is the next step in wound healing. Blood vessels in the injured area open up, allowing nutrients and oxygen to reach the wound. During this stage, white blood cells called macrophages are activated. They fight infection and release growth factors that promote tissue repair and regeneration.
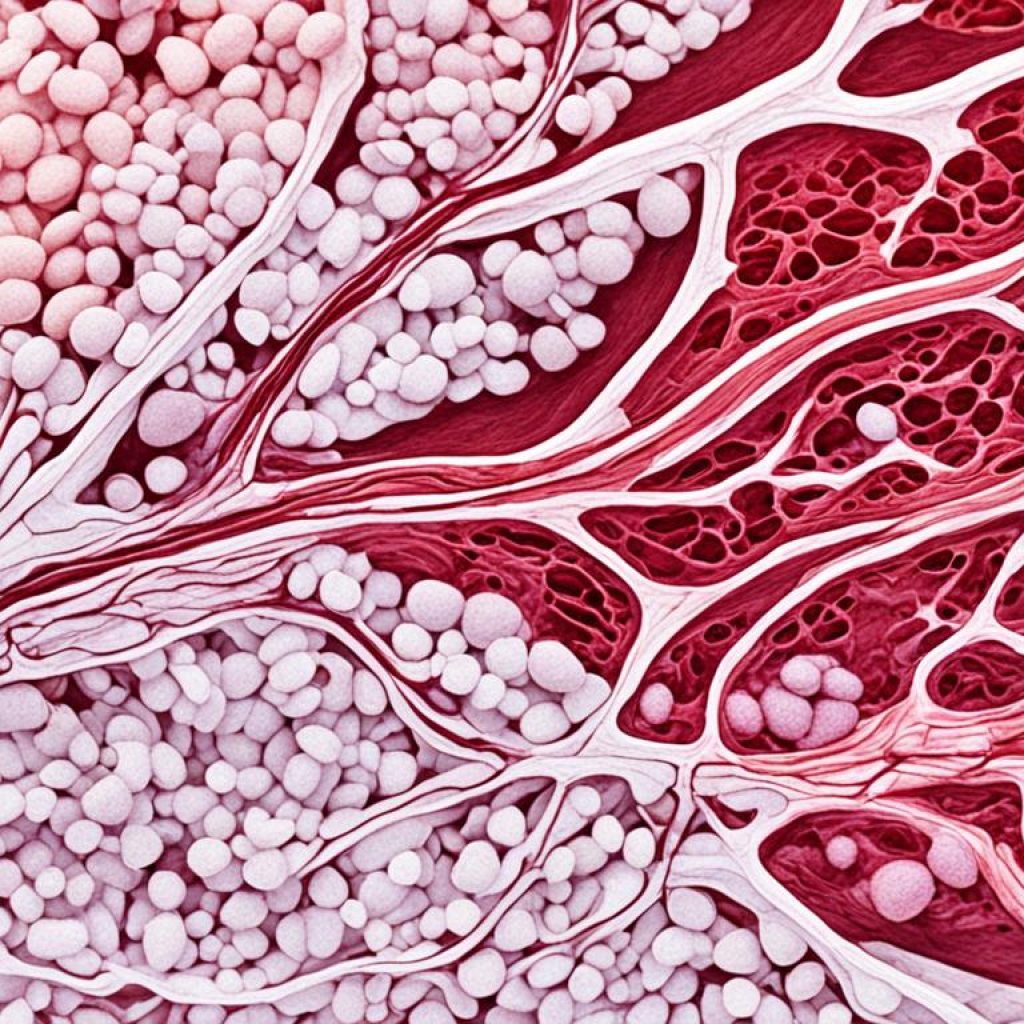
Growth and Rebuilding
Growth and rebuilding are essential stages of wound healing. Blood cells and collagen, a fibrous protein, are produced to create new tissue. This process helps close the wound and fill the gap, promoting proper healing and reducing the risk of infection. Collagen provides strength to the new tissue.
Strengthening
As the new tissue forms, it gradually strengthens over time. This strengthening phase of wound healing involves the alignment and organization of collagen fibers, making the wound more resistant to further injury. The wound’s strength increases as the tissues mature, helping to restore normal function.
It is important to note that the entire process of wound healing can take up to a couple of years to complete, depending on various factors such as the severity of the wound and the individual’s overall health.
Factors Affecting Wound Healing
While the wound healing process may seem straightforward, there are factors that can slow down or prevent healing entirely. One of the most significant factors is reduced or inadequate blood supply to the wound. Oxygen and nutrients carried by blood are essential for successful healing, and a lack of blood flow can significantly delay the healing process. This is particularly common in elderly individuals or those with conditions like diabetes, high blood pressure, obesity, or other vascular diseases. Smoking is also a significant risk factor for poor wound healing.
“Reduced or inadequate blood supply to the wound can significantly impair the healing process.”
If a wound is not healing within a reasonable time frame or shows signs of infection, it is important to seek medical attention to prevent complications. Chronic wounds, which are wounds that fail to heal within a typical time frame, are particularly challenging and often result from reduced blood supply. Identifying and addressing the underlying causes of poor blood supply is crucial for promoting successful healing.
Risk Factors for Poor Wound Healing:
- Reduced blood supply
- Elderly age
- Diabetes
- High blood pressure
- Obesity
- Smoking
- Vascular diseases
To illustrate the impact of reduced blood supply on wound healing, let’s take a closer look at chronic wounds: a significant consequence of poor blood circulation. Chronic wounds are wounds that fail to heal within a reasonable time frame, often persisting for months or even years. They pose a significant burden on patients’ quality of life and may lead to severe complications. Common types of chronic wounds include pressure ulcers, diabetic foot ulcers, and venous leg ulcers.
To highlight the prevalence and impact of chronic wounds, consider the following statistics:
| Type of Chronic Wound | Prevalence | Complications |
|---|---|---|
| Pressure Ulcers | 2.5 million cases annually in the United States (NPUAP, 2019) | Cellulitis, osteomyelitis, sepsis |
| Diabetic Foot Ulcers | Affecting approximately 15% of people with diabetes (CDC, 2021) | Cellulitis, osteomyelitis, lower limb amputation |
| Venous Leg Ulcers | 1–3% of the general population (Callam, 1992) | Cellulitis, dermatitis, deep vein thrombosis |
The impact of reduced blood supply in these chronic wounds is evident by the prolonged healing time and increased risk of complications. To prevent and manage chronic wounds, healthcare professionals must address the underlying risk factors, promote adequate blood flow, and implement appropriate wound care strategies. Timely interventions and comprehensive wound management can help reduce the burden of chronic wounds and improve patients’ overall quality of life.
Wound Management and Treatment
Proper wound management and treatment are essential for promoting optimal healing. The specific treatment approach will depend on the type and severity of the wound. Basic wound care involves cleaning the wound, applying an appropriate dressing, and keeping it clean and dry. In some cases, stitches or surgical closure may be necessary.
Wound healing time can vary depending on individual factors and the characteristics of the wound. It is essential to follow healthcare providers’ instructions and attend regular follow-up appointments to monitor the progress of the wound healing process effectively.

| Treatment | Description |
|---|---|
| Debridement | Removal of dead or infected tissue to promote healing |
| Topical dressings | Applying specialized dressings to protect the wound and facilitate healing |
| Wound irrigation | Flushing the wound with a sterile solution to remove debris and prevent infection |
| Negative pressure wound therapy | Using suction to promote wound healing and reduce bacterial contamination |
| Hyperbaric oxygen therapy | Administering high concentrations of oxygen to accelerate healing |
Key Points:
- Proper wound management includes cleaning, dressing, and keeping the wound clean and dry.
- Stitches or surgical closure may be necessary for certain wounds.
- Follow healthcare providers’ instructions and attend regular follow-up appointments.
“Effective wound management plays a critical role in promoting successful healing and preventing complications. By following recommended treatment protocols and adhering to healthcare providers’ instructions, individuals can optimize their recovery and achieve the best possible outcomes.”
Challenges in Wound Healing
Certain challenges can impede the wound healing process and lead to complications. One of the key challenges is reduced blood supply to the wound, which significantly hampers healing and may result in chronic wounds. Chronic wounds are particularly prevalent in individuals with comorbidities such as diabetes, high blood pressure, obesity, or vascular disease.
Chronic wounds:
Chronic wounds are wounds that do not heal within the expected timeframe of the normal healing process. These wounds often get stuck in the inflammatory phase and fail to progress to the next stages of healing. They can cause severe pain, reduce mobility, and negatively impact the quality of life for affected individuals.
Managing chronic wounds can be challenging and often requires specialized interventions. Healthcare providers may utilize advanced wound care techniques, such as wound dressings with growth factors or negative pressure therapy, to promote healing.
Another challenge in wound healing is infected wounds, which can significantly delay the healing process and increase the risk of systemic infections if left untreated.
Infected wounds:
Infected wounds occur when bacteria or other microorganisms enter the wound site and proliferate. Signs of wound infection may include increased pain, swelling, redness, warmth, or pus drainage. Prompt medical attention is crucial for managing infected wounds and preventing further complications.
By addressing challenges such as reduced blood supply, chronic wounds, and infected wounds, individuals can maximize their chances of successful wound healing. Seeking timely medical attention and following healthcare providers’ recommendations are key steps in managing these challenges and optimizing the healing process.
Historical Perspectives on Wound Healing
The understanding and management of wound healing have evolved over centuries, particularly in the context of military trauma care. In major conflicts, advancements in weapons technology, transportation, antiseptic practices, and surgical techniques have influenced how wounds are managed and treated. Surgeons have developed systems for rapid evacuation of the wounded from the battlefield and implemented strategies to optimize surgical care. Historical figures such as Baron Dominique-Jean Larrey and Florence Nightingale played significant roles in shaping modern military trauma care. These advancements in trauma care have also influenced civilian emergency medicine.

“The management of wounds has always been a matter of great interest in war.” – Baron Dominique-Jean Larrey
Advancements in Military Trauma Care
Through the course of history, there have been notable advancements in military trauma care that have revolutionized wound management and improved outcomes for injured soldiers. These advancements were driven by the urgent need to save lives on the battlefield and provide effective treatment for traumatic injuries.
| Advancement | Description |
|---|---|
| Antiseptic Practices | During the 19th century, the introduction of antiseptic practices by surgeons like Joseph Lister significantly reduced the risk of wound infections and improved healing outcomes. |
| Rapid Evacuation | Advancements in transportation, such as the introduction of field hospitals and medical evacuation systems, allowed injured soldiers to be quickly transported from the battlefield to receive specialized care. |
| Surgical Techniques | Surgeons developed innovative techniques, including the use of debridement to remove necrotic tissue and the use of skin grafts to facilitate wound closure and promote healing. |
These advancements in military trauma care paved the way for advancements in civilian healthcare as well, leading to improved wound management techniques and better outcomes in various medical settings.
The Role of Blood Supply in Wound Healing
Adequate blood supply is crucial for the successful healing of wounds. When a wound occurs, blood flow to the injured area increases, delivering essential oxygen and nutrients that are necessary for the healing process. Without an adequate blood supply, the healing process can be significantly hindered, leading to delayed wound healing and an increased risk of complications.
The presence of oxygen is particularly important in wound healing. Oxygen plays a vital role in various cellular activities that contribute to the repair and regeneration of damaged tissues. It helps stimulate the growth of new blood vessels, known as angiogenesis, which is essential for supplying oxygen and nutrients to the wound.
However, it is important to note that the balance of oxygen is critical in wound healing. Both too much and too little oxygen can have negative effects on the healing process. Excessive oxygen can lead to the formation of reactive oxygen species, which can cause tissue damage and impair the healing process. On the other hand, inadequate oxygen supply can slow down the healing process and increase the risk of infection.
Reduced blood flow to the wound, often caused by vascular diseases or other factors, can significantly delay the healing process. It limits the delivery of oxygen and nutrients to the wound, impeding the body’s natural healing mechanisms. Additionally, a compromised blood supply can weaken the immune response, making the wound more susceptible to infections.
To optimize wound healing and minimize the risk of further complications, it is crucial to address any issues related to blood supply. This may involve improving overall cardiovascular health, managing underlying conditions that affect blood flow, and promoting proper wound care techniques to enhance blood circulation.
Key Takeaways:
- Adequate blood supply is vital for successful wound healing.
- Oxygen and nutrients carried by the blood are necessary for the healing process.
- The right balance of oxygen is crucial, and both too much and too little can hinder healing.
- Reduced blood flow to the wound can significantly delay the healing process and increase the risk of complications.
- Addressing issues with blood supply can optimize wound healing and minimize the risk of further complications.
Contemporary Practices in Wound Healing
In modern medicine, significant advancements in wound healing techniques and treatments have emerged. These advancements aim to optimize the healing process, reduce complications, and enhance outcomes for patients.
Current wound care treatments encompass a range of innovative approaches tailored to each individual’s unique needs and the specific characteristics of the wound. These treatments may include:
- Specialized Dressings: Advanced dressings, such as hydrogels or foams, are designed to create an optimal wound healing environment by maintaining moisture levels, managing exudate, and promoting tissue regeneration.
- Growth Factors: Biologically active proteins can be applied to wounds to stimulate cell migration, proliferation, and differentiation, accelerating the healing process.
- Antimicrobial Agents: Topical antimicrobial agents, such as silver-based products or antimicrobial dressings, are used to prevent or treat wound infections, reducing the risk of complications.
- Advanced Wound Closure Techniques: Innovative closure methods, including negative pressure wound therapy or surgical offloading devices, provide effective wound closure, allowing for better healing outcomes.
Healthcare providers play a crucial role in collaborating with patients to develop individualized treatment plans based on these advancements. By staying up-to-date with the latest developments in wound healing, healthcare providers can offer the best care and support to their patients.
Let’s take a look at a table highlighting some contemporary wound healing advancements:
| Advancements | Benefits |
|---|---|
| Specialized Dressings | Optimize wound environment, promote tissue regeneration |
| Growth Factors | Accelerate cell migration and proliferation |
| Antimicrobial Agents | Prevent and treat wound infections |
| Advanced Wound Closure Techniques | Facilitate effective wound closure |
The Importance of Timely Medical Attention
Timely medical attention is crucial for effective wound care and optimal healing. When dealing with wounds, it is essential to seek medical assistance promptly to prevent complications and ensure appropriate treatment. If a wound is not healing within a reasonable time frame or shows signs of infection, it is particularly important to seek immediate medical attention.
Signs of infection in a wound may include:
- Increased swelling
- Redness
- Warmth
- Pain
- Pus drainage
Delayed wound healing can lead to further complications and may require more aggressive interventions. By seeking timely medical attention, individuals can receive the necessary treatment and support for their wound healing process.
Conclusion
The process of wound healing is a remarkable and intricate series of events that the body undergoes to repair itself after an injury. By understanding the stages of wound healing and the factors that can impact the healing process, individuals can take proactive steps to optimize their recovery and minimize the risk of complications.
Proper wound management is essential for successful healing. This includes cleaning the wound, applying appropriate dressings, and following healthcare providers’ instructions for wound care. Timely medical attention is crucial, especially if a wound shows signs of infection or is not healing within a reasonable timeframe.
Key takeaways on wound healing include the importance of adequate blood supply, the role of inflammation in the repair process, and the impact of individual factors on healing time. By staying informed about advancements in wound care treatments and following healthcare providers’ recommendations, individuals can support their body’s natural healing mechanisms and promote optimal wound healing.
FAQ
How do wounds actually heal on the body?
Wounds heal through a complex process involving several stages. The steps include stopping the bleeding, inflammation, growth and rebuilding of new tissue, and strengthening of the healed wound.
What are the stages of wound healing?
The stages of wound healing include hemostasis (stopping the bleeding), inflammation, growth and rebuilding of new tissue, and strengthening of the healed wound.
What is the appropriate wound care treatment?
The specific treatment approach for wounds depends on the type and severity of the wound. Basic wound care involves cleaning the wound, applying appropriate dressings, and keeping it clean and dry. In some cases, stitches or surgical closure may be necessary.
What factors can affect wound healing?
Reduced blood supply, chronic wounds, and certain risk factors like diabetes, high blood pressure, obesity, and smoking can slow down or prevent proper wound healing.
How long does wound healing take?
The time required for wound healing varies depending on individual factors and the characteristics of the wound. In general, the entire healing process can take up to a couple of years to complete.
What challenges are associated with wound healing?
Reduced blood supply, chronic wounds, and infected wounds can significantly hinder the wound healing process and increase the risk of complications.
How has wound healing evolved over time?
Advancements in military trauma care, including weapons technology, transportation, antiseptic practices, and surgical techniques, have influenced how wounds are managed and treated. Historical figures like Baron Dominique-Jean Larrey and Florence Nightingale played significant roles in shaping modern military trauma care.
What is the role of blood supply in wound healing?
Adequate blood supply is vital for successful wound healing, as oxygen and nutrients carried by the blood are essential for the healing process. Reduced blood flow can significantly delay healing and increase the risk of complications.
What are the contemporary practices in wound healing?
Current wound care treatments may involve the use of specialized dressings, growth factors, antimicrobial agents, and advanced wound closure techniques to optimize the healing process and enhance outcomes.
How important is timely medical attention for wound healing?
Timely medical attention is essential for effective wound care and optimal healing. If a wound is not healing within a reasonable time frame or shows signs of infection, seeking medical attention promptly can prevent complications and ensure appropriate treatment.
fighters can optimize their recovery and minimize the risk of complications. understanding how do wounds actually heal on the body - for fighters wound healing is a remarkable process that the body undergoes to repair itself after an injury. it involves a series of complex steps that work together to prom
Last modified: March 11, 2024